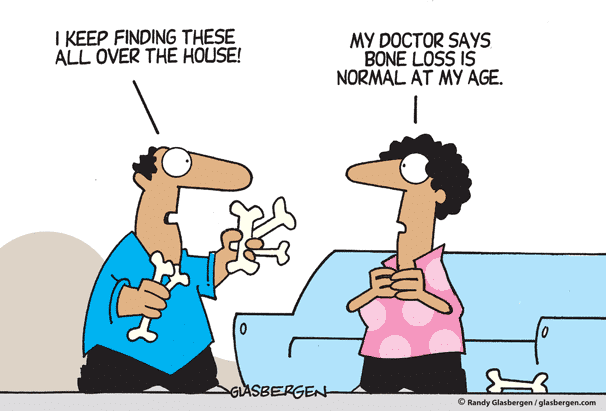
Calcium supplements: How much is enough? Can you get too much?
Like many of you, I’ve been advised to take calcium supplements.
With health insurance what it is (and was when my employer provided health insurance), every couple of years my company would change coverage, and I’d have to change doctors to stay in “network.” As I aged into my 50s and started getting bone density exams, I received a number of vague recommendations from said doctors to “take calcium.”
I’d have to change doctors to stay in “network.” As I aged into my 50s and started getting bone density exams, I received a number of vague recommendations from said doctors to “take calcium.”
But recently a reader (thank you, Eric!) sent me an article that reviewed an important study showing that calcium and vitamin D supplements may not protect against bone fractures. The meta-analysis, published in JAMA, analyzed 33 randomized clinical trials involving more than 50,000 “free living” adults (not in nursing homes, hospitals, or other facilities) over age 50. The data was convincing: supplementing with calcium and vitamin D did not show any clear benefit, regardless of the dose, gender, history of fractures, or calcium in the diet.
However, we do need calcium, and we do need vitamin D.
The Washington Post, in reporting on this study, quotes Marion Nestle, professor emerita of food sciences and nutrition at New York University, who said bone health involves many different aspects of eating and activity. And it’s not just what you eat that influences bone health – it’s lifestyle.
 The Post quotes Nestle as cautioning clinicians “to think carefully before advising calcium and vitamin D supplementation for healthy individuals.” Lifestyle factors influence bone health, and health in general. “Bone preservation throughout life requires eating healthfully, engaging in weight-bearing activity (walking, running, dancing), avoiding excessive alcohol, and not smoking.”
The Post quotes Nestle as cautioning clinicians “to think carefully before advising calcium and vitamin D supplementation for healthy individuals.” Lifestyle factors influence bone health, and health in general. “Bone preservation throughout life requires eating healthfully, engaging in weight-bearing activity (walking, running, dancing), avoiding excessive alcohol, and not smoking.”
Facts
Calcium is a mineral, necessary for building and maintaining strong bones, but it’s also important for just about every bodily function: a critical component of blood clotting, nerve messaging, and to help release hormones and enzymes.
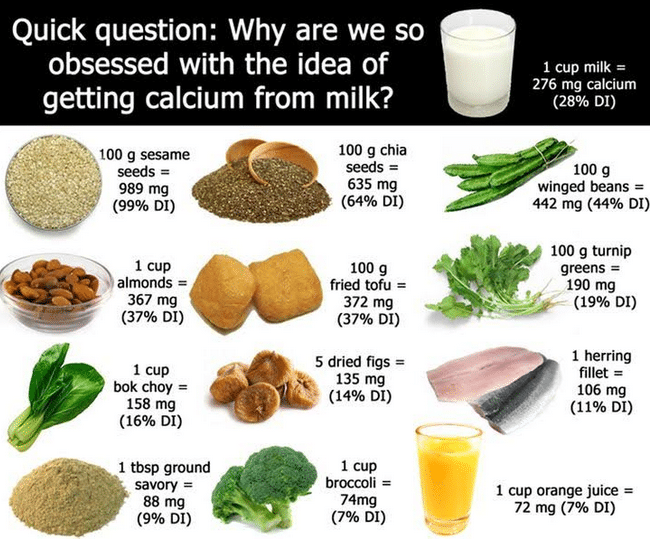
Calcium is found in many foods, and it’s stored in bones and teeth, where it supports structure and hardness. The body utilizes calcium by releasing the stored mineral through bone remodeling — the process by which bone is constantly broken down and rebuilt.
Inadequate calcium intake influences bone loss and the risk for osteoporosis, or thinning of bones. Also, hypertension and colorectal cancer may be linked to low calcium intake.
Article continues below graphic.
 How Much Is Enough?
How Much Is Enough?
Studies show that certain groups of people do NOT get the recommended amounts of calcium from the foods they eat. These include:
Boys 9 to 13
Girls 9 to 18
Women older than 50
Men older than 70
Postmenopausal women are at higher risk for bone loss: due to a decrease in estrogen production after menopause, they are less able to retain dietary calcium.
And although age and sex influences the amount of calcium recommended daily, there’s controversy about how much is actually enough.
The Institute of Medicine recommends all adults 19-15 years and adult men 51-70 obtain (through diet and supplements)1,000 mg daily; adult women 51-70, and all adults 71 years and older 1200 mg. However, Dr. Walter Willet, chair of the Department of Nutrition at Harvard T.H. Chan School of Public Health notes that other health organizations recommend much less. He says, “Essentially, I think that adults do not need 1,200 mg of calcium a day. The World Health Organization’s recommendation of 500 mg is probably about right. The United Kingdom sets the goal at 700 mg, which is fine too. It allows for a little leeway.”
It’s pretty easy to eat 700 mg of dietary calcium daily. However, our bodies are pretty complicated, and work like a symphony orchestra, with many musicians playing different instruments, sometimes at differing tempos, all contributing different sounds and structures to the harmonious whole.
And so, calcium, while essential, works in concert with vitamin D and other micronutrients like magnesium and vitamin C to be absorbed.
 Vitamin D, acquired both through sunlight and diet (and supplements) is the most important nutrient for calcium absorption. Vitamin D is found in eggs, fatty fish, and liver. Foods rich in magnesium plus other essential vitamins and minerals and that aid the absorption of calcium (some contain calcium!) are almonds, avocado, cashews and Brazil nuts, flax and sesame seeds, spinach, Swiss chard, and tuna.
Vitamin D, acquired both through sunlight and diet (and supplements) is the most important nutrient for calcium absorption. Vitamin D is found in eggs, fatty fish, and liver. Foods rich in magnesium plus other essential vitamins and minerals and that aid the absorption of calcium (some contain calcium!) are almonds, avocado, cashews and Brazil nuts, flax and sesame seeds, spinach, Swiss chard, and tuna.
Calcium-rich foods include dairy, especially yogurt, some leafy greens like kale and broccoli, fish with soft, edible bones like canned sardines and salmon, and fortified foods, including breakfast cereals, juices, soy and rice beverages, and tofu.
Just think: We in Cuenca have a huge variety of fresh fruits and vegetables that are rich in potassium, magnesium, vitamin C and beta-carotene, all contributing to a higher bone mass.
Some foods can interfere with absorption. Foods rich in phytic acid (wheat bran, legumes, seeds, nuts, and soy isolates) and oxalic acid (spinach, collard greens, sweet potatoes, rhubarb, and beans) may bind to calcium and inhibit absorption.
For example, some research shows that eating spinach and milk at the same time can reduce the absorption of calcium from milk. However, eating a variety of foods throughout the day is recommended to create a dietary milieu that enhances overall nutrition, and as long as you’re not overdoing on the phytates or oxalic acid it does not appear that combining foods has a negative effect on absorption. But, eat whole foods, instead of nutrients or processed foods. Eat whole wheat bread, but don’t add processed wheat bran to your breakfast.
By the way, high sodium diets reduce calcium absorption — another reason to avoid salting your food and consuming excessive packaged and processed foods. When dining out, consider that soups and sauces are especially high in salt.
Can You Get Too Much?
Maybe. But not typically from your diet. Although a well-publicized 2016 study cautioned women against taking calcium supplements because of a higher risk for heart disease, the University of California’s Berkeley Wellness newsletter says that “observational studies and clinical trials have yielded inconsistent though mostly reassuring results about the safety of calcium supplements.”
Article continues below graphic.
 They conclude, “It’s best to get calcium from your diet because foods naturally rich in calcium supply many nutrients important for bones and general health. In addition, high doses of calcium supplements increase the risk of the most common type of kidney stones in some people, while foods naturally rich in calcium (notably dairy products) protect against stones. If you can’t get the recommended 1,000 to 1,200 milligrams of calcium a day from diet alone, you may need only a small amount of supplemental calcium to fill the gap. More is not necessarily better.”
They conclude, “It’s best to get calcium from your diet because foods naturally rich in calcium supply many nutrients important for bones and general health. In addition, high doses of calcium supplements increase the risk of the most common type of kidney stones in some people, while foods naturally rich in calcium (notably dairy products) protect against stones. If you can’t get the recommended 1,000 to 1,200 milligrams of calcium a day from diet alone, you may need only a small amount of supplemental calcium to fill the gap. More is not necessarily better.”
Foods Rich In Calcium Milligrams (mg) per serving
Yogurt, plain, low fat, 8 oz. 415
Mozzarella cheese, part skim, 1 ½ oz. 333
Sardines, canned in oil, with bones, 3 oz. 325
Milk, reduced-fat (2%), 8 oz. 293
Orange juice, calcium-fortified, 6 oz. 261
Tofu, firm, made with calcium sulfate, ½ cup 253
Salmon, pink, canned, solids with bones, 3 oz. 181
Ready-to-eat cereal, calcium-fortified, 1 cup 100-1000
Kale, fresh, cooked, 1 cup 94
Bok choi (Chinese cabbage), raw, shredded, 1 cup 74
Tortilla, corn, 6” diameter 46
Tortilla, flour, 6” diameter 32
Bread, whole-wheat, 1 slice 30
Kale, raw, chopped, 1 cup 24
Broccoli, raw, ½ cup 21
According to Dr Andrew Weil, people who have osteopenia (low bone mineral density) have a greater chance of developing osteoporosis, a condition where bones are weak and fractures can occur. In both men and women, this could be because of poor dietary consumption, or metabolism issues that don’t allow absorption such as pancreatitis, celiac disease, or inflammatory bowel disorders such as Crohn’s disease or ulcerative colitis. Chemotherapy, radiation, or medications such as steroids to treat a variety of conditions, such as asthma, can contribute to bone thinning.
Aging, being thin, having a family history of osteoporosis, being Caucasian or Asian, lack of physical activity, smoking, and excessive alcohol raises risk.
A diet low in calcium and vitamin D is a pretty big risk factor for thinning bones. And your diet is one of the easiest one to change. You can’t change your age, your sex, your race, or your family history.
But the good news is you can eat a diet rich in calcium and vitamin D, get out your walking shoes, do some resistance training to strengthen your bones and tendons, and enjoy your good health while lowering your risk.
How much calcium are you consuming? Just use this online calculator to find out!
https://bcdairy.ca/nutritioneducation/calciumcalculator/
Sources
Berkeley Wellness. Calcium Pills: Heartening News. http://www.berkeleywellness.com/supplements/minerals/article/calcium-supplements-heartening-news
Dr. Andrew Weil. Health & Wellness—Bone & Joint. Osteopenia. https://www.drweil.com/health-wellness/body-mind-spirit/bone-joint/osteopenia/
Harvard Health Letter. How much calcium do you really need?https://www.health.harvard.edu/staying-healthy/how-much-calcium-do-you-really-need
Journal of the American Medical Association. Association Between Calcium or Vitamin D Supplementation and Fracture Incidence in Community-Dwelling Older Adults. A Systematic Review and Meta-analysis. https://jamanetwork.com/journals/jama/article-abstract/2667071?redirect=true
National Institutes of Health, Office of Dietary Supplements: Calcium Fact Sheet for Consumers. https://ods.od.nih.gov/factsheets/Calcium-Consumer/
The Washington Post. Calcium and vitamin D supplements may not protect against bone fractures.https://www.washingtonpost.com/news/to-your-health/wp/2017/12/26/calcium-and-vitamin-d-supplements-may-not-protect-against-bone-fractures-in-elderly/?utm_term=.1305436e0abc