Is there a ‘cure’ for type 2 diabetes? One man’s journey from ‘at risk’ to ‘in remission’
Susan’s note: As reported in the journal Endocrine Reviews, the treatment of obesity continues to be a major challenge. Obesity is now pandemic in the United States as well as in other nations. In the United States, it is now more common to be overweight than not; over two-thirds of the population meet the criteria and over one third are obese.
Although diet and exercise are traditionally the first recommendations for the treatment of obesity, for most individuals, this behavioral modification is not sustained — most people who “go on” a diet regain the weight, and often more.
As noted, “Given this relatively bleak picture, it is not surprising that bariatric surgery has increased in popularity due to its ability to produce long-term weight loss that is superior to traditional weight loss treatments in both magnitude and durability. Studies show that some bariatric procedures reduce overall mortality despite the inherent risks of the surgery itself — and research is ongoing to understand what are the long-term metabolic benefits.”
Bariatric surgery (bariatrics is the branch of medicine that deals with the study and treatment of obesity) dates back to 1954 with a procedure called a jejunoileal bypass. However, the complications of this open procedure were dire, including severe diarrhea and dehydration.
Current bariatric surgery techniques are light years beyond the first draconian procedures, and include a variety of procedures, often performed laparoscopically, including the gastric band, to reduce the size of the stomach; the removal of a portion of the stomach (sleeve gastrectomy or biliopancreatic diversion with duodenal switch); or by resecting and re-routing the small intestine to a small stomach pouch, known as gastric bypass surgery.
Today’s Guest Columnist, Jeff Schinsky, shares his personal journey from suffering complications of type 2 diabetes to reversing the symptoms of the disease and losing a significant amount of weight. More about the studies on the efficacy and safety of gastric bypass follows Jeff’s personal story.

By Jeff Schinsky
I was obese, and I had type 2 diabetes. And yes, I thought I was “pretty” good with my diet, but I continued to gain weight. Eventually, I found myself on three different oral meds and long-acting insulin. I didn’t realize it then, but I was eating far more than I thought I was.
Today, I can only eat about the equivalent of a single cup of food at any one sitting. Or, about the amount of food represented by a medium-sized banana. A little over four months ago I had a procedure known as a “mini-gastric bypass.”
If you’ve heard of the Roux-en-Y procedure, there are similarities. I had it done at the IESS hospital here in Cuenca, so it didn’t cost me anything. If you paid out of pocket to have the surgery at, say, Monte Sinai, I believe it costs around $5,000.
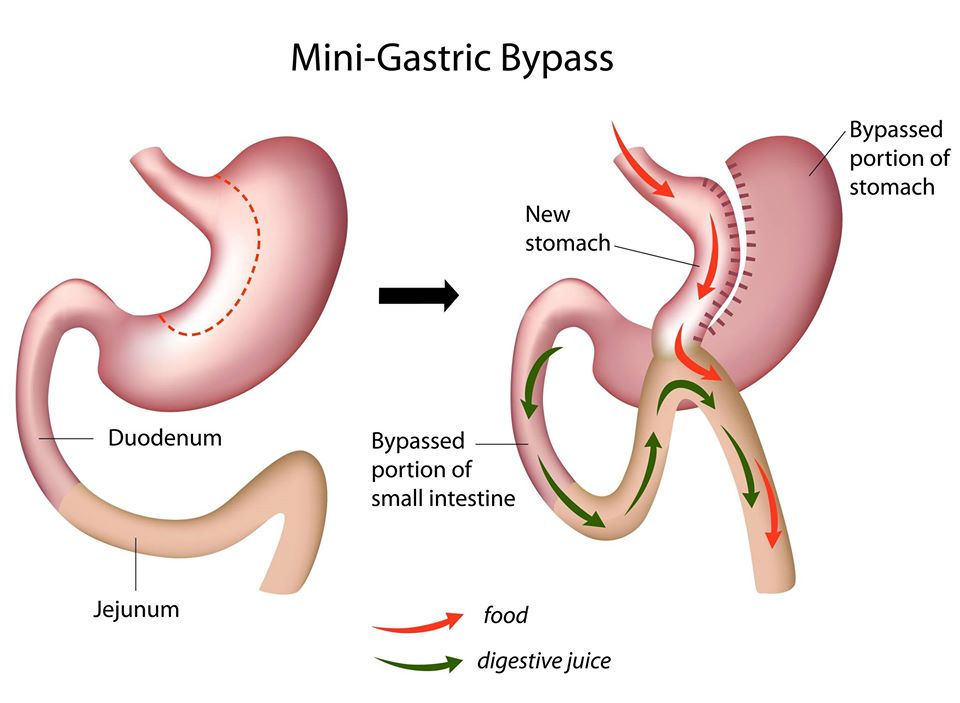
The Mini-Gastric Bypass or single anastomosis gastric bypass, is an effective and well-established procedure which combines some of the properties of a gastric sleeve and a standard gastric bypass. The upper part of the stomach is divided into a tube, similar to the top three quarters of a sleeve, and then joined to a loop of intestine.
I was surprised but excited that they offered this type of surgery. It sure does make a lot of sense, though — it’s far less expensive to cover medical care for a relatively healthy person than it does to have to treat someone whose body is being ravaged by type 2 diabetes. The bariatric surgery program at IESS is fairly busy, and I know of at least three surgeons there who perform a variety of bariatric surgeries.
You have to prepare very thoroughly for surgery through this program. But that is what makes it successful. You don’t sign up one day, and then go for surgery the next; it took me a little over a year to lose the requisite 10 percent of my weight — this is a requirement for all patients. You have to lose to prove that you can stick to a reasonable diet after the surgery. And as my doctor said, losing weight also makes the surgery easier and less risky.
During that year, I had monthly visits with the nutritionist, a psychologist, and an endocrinologist. Closer to the surgery date, I was thoroughly, physically evaluated by just about every medical discipline represented at the hospital to prove yourself to be a good overall “risk” for having a favorable outcome. During this time the experts also determined which type of surgery they would perform, as some are better suited to different individuals.
The mini-gastric bypass surgery has been shown to give me the best chance of putting my diabetes into remission. Check out the diagram of what they did to me below, or click here for more details.
When I entered the program at IESS, my BMI was 40.2: I weighed 272 pounds and I’m 5 feet nine inches. I was 61 at the time and had diabetes for about seven or eight years.

Jeff Schinsky: Reversing symptoms of type 2 diabetes means ‘normal’ blood glucose and a radical change in eating behaviors.
I suffer from peripheral neuropathy in my feet, and I was having other nerve-related issues, not to mention high blood pressure. But otherwise — believe it or not — I was in pretty good shape! This surgery is not an easy procedure and the doc only agreed to do it because of my diabetes. I managed to get down to 235 by my surgery date, and then on the 5th of August 2019, I went under the knife. The doc projected that it would take about three to four hours, but mine was a little trickier and ended up taking close to five hours.
In case you’re wondering, the surgery itself isn’t very painful. It’s done laparoscopically, and I ended up with five small incisions, each about half-inch wide. What was painful after the surgery was from the gas they pump you full of to inflate your abdomen and make it easier for the surgeon to maneuver. But after a few days of walking a lot and trying a few other strategies, the gas finally dissipated. Residual pain was easily controlled with over-the-counter pain medications.
In the first month, I lost 35 pounds almost immediately. Then for two more months —nothing. Then I suddenly lost 10 more pounds. Then for nearly two more months — nothing. I have started losing again, and I’m currently down to 185. My blood sugar is normal now! My A1c [The A1c test evaluates the average amount of glucose in the blood over the last two to three months by measuring the percentage of glycated hemoglobin in the blood] from last week was 5.5%. Best yet, I take no diabetes meds anymore, nor am I taking blood pressure meds. My diabetes is in remission! I’ve gone from my largest waist size of 44 inches, down to a 34/36. My biggest problem right now is that I have almost no clothing that fits me. But hey, what a problem to have! You can get an idea of how I’ve changed since the surgery in the photos below.
One thing you need to know about this surgery is that it is absolutely not the “easy way out.” It requires a commitment to a whole new way of living, eating, and thinking about food. Many of the things I loved before, I can no longer eat. Some because I don’t digest them well, and some because they don’t taste the same to me as they did before the surgery. Also, recovery can be very challenging. Right up until recently, I stayed nauseous most of the time. Pretty much all foods made me feel ill to some extent, but at least I wasn’t vomiting or otherwise suffering. I’ll also have to take a handful of supplements for at least the first couple of years, if not the rest of my life. I’m eating (and enjoying) a wider variety of foods now, but in very small quantities.
And you don’t just lose fat. You lose muscle, too, and you gain extra folds of skin in places you’d rather not have it. Of course, Cuenca is a cheap place for a tummy-tuck, so it could be worse. The important thing, however, is that my diabetes and my blood pressure problems are in remission, and I can regain much of the muscle I lost. Another side effect of the surgery for most folks (including myself) is that the shock to your body causes a change in your hair’s growth cycle, so many people go through a period where their hair thins out significantly — but it almost always grows back! (So I’ve read.)
Obviously, this surgery isn’t for everybody. Depending on your overall health, you may not even qualify for the surgery. However, it is indeed a legitimate and reasonable step to take for someone struggling with type 2 diabetes.
Now, if you’re thinking that you should wait until things get “really bad” before you consider bariatric surgery, that’s a huge mistake in a number of ways. Susan shared an article with me written by Ted Kyle, founder of ConscienceHealth.org [an organization that “exists to help experts and organizations work for sound approaches to health and obesity”].
“…the data has been clear for some time now. Bariatric surgery is not a last resort. It’s a most effective treatment for people who need it. We would not encourage someone with heart disease or cancer to wait until they’re desperate to opt for an effective treatment. We encourage them to do whatever it takes to reclaim good health.”
So bariatric surgery isn’t the only solution, but it can be a solution for a lot of people. For me, it did the trick! I wouldn’t dare make any predictions for anyone else, but as you’ll read in the article referenced above, the odds of bariatric surgery putting your diabetes into remission diminishes the longer you’re actively diabetic and taking a lot of meds/insulin to control your disease.
In any case, I hope I’ve given you something to think about. It’s not an easy path, but I’m finding it worthwhile, and I’m thinking I’ve just added a number of years onto my life. More time with my family. More time, able to function under my own steam (with my own limbs). More of everything — except complications from diabetes and all the bad things that go with it. Cheers!
____________________
Jeff Schinsky relocated to Cuenca from Colorado in 2014, and is the lead administrator of the Facebook group “Expats Without Agendas.” Jeff lives with his wife Annie, their three daughters, and their dog Sisko
Note: According to the American Society for Metabolic and Bariatric Surgery, type 2 diabetes is a leading cause of death in the U.S. and is a major contributor to morbidity and mortality from heart disease, stroke and kidney failure. Each year millions of individuals die from the effects of T2DM. With the advancements in bariatric surgery, many of these individuals could be saved and experience an improved quality of health and life.
While bariatric surgery certainly has some risk, the long-term risk of continued diabetes (which is often inadequately treated with medication) typically outweighs the risk of a surgical procedure for most patients. Each patient’s individual risks for surgery, though, should be evaluated in the context of the duration and severity of their diabetes as well as their other obesity-related health problems.
Surgery improves type 2 diabetes in nearly 90 percent of patients by:
- lowering blood sugar
- reducing the dosage and type of medication required
- improving diabetes-related health problems
Surgery causes type 2 diabetes to go into remission in 78 percent of individuals by:
- reducing blood sugar levels to normal levels
- eliminating the need for diabetes medications
Health Improvements
- Cause the improvement or remission of T2DM to last for years
_______________________
Sources:
American Society for Metabolic and Bariatric Surgery. Surgery for Diabetes.
ConscienHealth.org. Last resort: a false premise for bariatric surgery.
Porto Biomedical Journal. A brief history of bariatric surgery.
Endocrine Reviews. All Bariatric Surgeries Are Not Created Equal: Insights from Mechanistic Comparisons.