Osteoporosis: Is it a ‘woman’s disease’ or can men get it too?
Like many of you, I’ve been advised to take calcium supplements.
As I aged into my 50s I received a number of vague recommendations from doctors to “take calcium” after a bone density exam showed bone loss.
People who have osteopenia (low bone mineral density) have a greater chance of developing osteoporosis, a condition where bones are weak and fractures can occur.
But taking supplemental calcium and vitamin D may not protect against bone fractures.
A 2017 meta-analysis analyzed 33 randomized clinical trials involving more than 50,000 “free-living” adults (not in nursing homes, hospitals, or other facilities) over age 50. The data was convincing: supplementing with calcium and vitamin D did not show any clear benefit, regardless of the dose, gender, history of fractures, or calcium in the diet.
And a more recent 2018 meta-analysis analyzed 25 randomized controlled trials of 43,510 participants and also found that regular supplementation with calcium, vitamin D or both was not found to be better than placebo to reduce the risk of fracture.
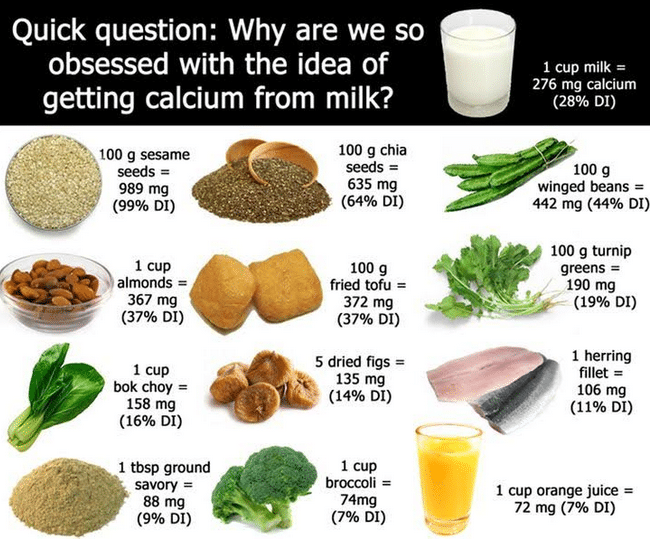
However, we do need calcium, and we do need vitamin D. But it’s best to get it from your diet.
And it’s not just diet that keeps bones healthy! More below.
Do men get osteoporosis, or just women?
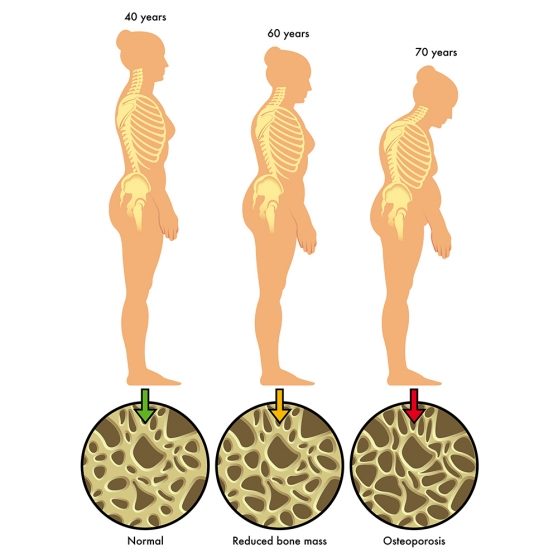
According to the International Osteoporosis Foundation, one in five men over age 50 will have an osteoporosis-related fracture — which is greater than the likelihood of developing prostate cancer! Men in their fifties do not experience the rapid loss of bone mass that women do after menopause, but by age 65 or 70 both men and women lose bone mass at the same rate and the absorption of calcium decreases in both sexes.
Because men are pretty advanced in age when they experience that first fracture, they are more likely to suffer serious consequences or even death.
 Facts about bone health
Facts about bone health
Calcium is necessary for building and maintaining strong bones, but it’s also important for just about every bodily function: a critical component of blood clotting, nerve messaging, and to help release hormones and enzymes.
All but one percent of calcium is found in the blood, extracellular fluid, and other tissues, where it plays a vital role in vasodilation, muscle contraction, nerve transmission, and glandular secretions — only one percent is stored in the bones. The body utilizes calcium by releasing the stored mineral through bone remodeling — the process by which bone is constantly broken down and rebuilt.
How Much Is Enough?
Studies show that certain groups of people do not get the recommended amounts of calcium from the foods they eat. These include:
- Boys 9 to 13
- Girls 9 to 18
- Women older than 50 — Postmenopausal women are at higher risk for bone loss — they are less able to retain dietary calcium due to a decrease in estrogen production after menopause.
- Men older than 70
The Institute of Medicine recommends all adults 19-15 years and adult men 51-70 obtain (through diet and supplements) 1,000 mg daily; adult women 51-70, and all adults 71 years and older 1200 mg.
But Dr. Walter Willet, chair of the Department of Nutrition at Harvard T.H. Chan School of Public Health notes that other health organizations recommend much less. He says, “Essentially, I think that adults do not need 1,200 mg of calcium a day. The World Health Organization’s recommendation of 500 mg is probably about right. The United Kingdom sets the goal at 700 mg, which is fine too. It allows for a little leeway.”
 Can You Get Too Much?
Can You Get Too Much?
Maybe. But not typically from your diet. Although a well-publicized 2016 study cautioned women against taking calcium supplements because of a higher risk for heart disease, the University of California’s Berkeley Wellness Newsletter says that “observational studies and clinical trials have yielded inconsistent though mostly reassuring results about the safety of calcium supplements.”
They conclude, “It’s best to get calcium from your diet because foods naturally rich in calcium supply many nutrients important for bones and general health. Importantly, high doses of calcium supplements increase the risk of the most common type of kidney stones in some people, while foods naturally rich in calcium (notably dairy products) protect against stones.
If you can’t get the recommended 1,000 to 1,200 milligrams of calcium a day from diet alone, you may need only a small amount of supplemental calcium to fill the gap. More is not necessarily better.”
Most people can easily consume at least 700 mg of dietary calcium daily — because we eat food, not nutrients.
And food sources are much greater than the sum of its parts because we absorb calcium in concert with vitamin D and other micronutrients like magnesium and vitamin C.
Calcium-rich foods include dairy, especially yogurt, some leafy greens like kale and broccoli, fish with soft, edible bones like canned sardines and salmon, and fortified foods, including breakfast cereals, juices, soy and rice beverages, and tofu.
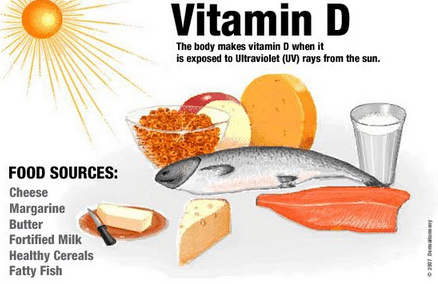
Vitamin D, acquired both through sunlight and diet (and supplements) is the most important nutrient for calcium absorption. Good food sources of vitamin D include eggs, fatty fish, and liver. |
Foods rich in magnesium plus other essential vitamins and minerals are necessary for the absorption of calcium — and some contain calcium — include almonds, avocado, cashews, and Brazil nuts, flax and sesame seeds, spinach, Swiss chard, and tuna.
 What else can you do to promote your calcium absorption?
What else can you do to promote your calcium absorption?
- Decrease your sodium intake. Avoid salty processed foods and fast food. Don’t salt your food before tasting it.
- Some foods can inhibit calcium absorption too. Foods rich in phytic acid (wheat bran, legumes, seeds, nuts, and soy isolates) and oxalic acid (spinach, collard greens, sweet potatoes, rhubarb, and beans) may bind to calcium and inhibit absorption. But don’t avoid these foods… instead…
- Eat a variety of foods throughout the day to create a dietary milieu that enhances overall nutrition. As long as you’re not overdoing on the phytates or oxalic acid it does not appear that combining foods has a negative effect on absorption.
- Eat your fruits and veggies
Fruits and vegetables are the best sources of potassium, magnesium, vitamin K, vitamin C and beta-carotene. Skip the raw kale smoothies — raw kale, spinach, chard and beet greens have significant amounts exalic acid (especially raw and in the amounts used to make smoothies) and can reduce calcium absorption. - Limit caffeine intake. Get some sun every day — not too much, especially here in Cuenca, where we’re so close to the sun. Depending on your sensitivity and other risk factors, about 10 – 30 minutes of midday sun daily. Sun and vitamin D is the subject of another column! Read more here.
- Drink moderately (one drink per day for women/two for men) — chronic and heavy drinking can suppress new bone formation.
- Increase weight-bearing activities like walking, jogging, or dancing and muscle-strengthening exercises like working with weights or resistance bands to build and maintain bone density. Try to do at least 30 minutes of exercise on most days of the week.
 Here in Cuenca we enjoy a huge variety of fresh fruits and vegetables that are rich in potassium, magnesium, vitamin C and beta-carotene, all contributing to a higher bone mass.
Here in Cuenca we enjoy a huge variety of fresh fruits and vegetables that are rich in potassium, magnesium, vitamin C and beta-carotene, all contributing to a higher bone mass.
And we’re in a walking city! Get out your walking shoes, bring along your resistance band and do some resistance training to strengthen your bones and tendons — at the same time, you’ll get some vitamin D. Enjoy your good health while lowering your risk for osteoporosis.
Some risk factors you can change, and others you cannot. You cannot change your age, your sex, your family history, or your race – Caucasians and Asians have a higher risk of developing osteoporosis.
But you can change important risk factors. You can change your diet, get daily weight-bearing activity, stop smoking, and not drink excessively.
How much calcium are you consuming? Have some fun! Click here to see how much calcium you’re consuming today and if it’s not enough just drag and drop some foods into the calculator to plan for a better calcium day tomorrow.
| 25 foods high in calcium | ||
| Produce | Serving size | Estimated calcium in milligrams |
| Collard greens, frozen | 8 oz | 360 |
| Broccoli rabe | 8 oz | 200 |
| Kale, frozen | 8 oz | 180 |
| Soy Beans, green, boiled | 8 oz | 175 |
| Bok Choy, cooked, boiled | 8 oz | 160 |
| Figs, dried | 2 figs | 65 |
| Broccoli, fresh, cooked | 8 oz | 60 |
| Oranges | 1 whole | 55 |
| Seafood | Serving size | Estimated calcium |
| Sardines, canned with bones | 3 oz | 325 |
| Salmon, canned with bones | 3 oz | 180 |
| Shrimp, canned | 3 oz | 125 |
| Dairy | Serving size | Estimated calcium |
| Ricotta, part-skim | 4 oz | 335 |
| Yogurt, plain, low-fat | 6 oz | 310 |
| Milk, skim, low-fat, whole | 8 oz | 300 |
| Yogurt with fruit, low-fat | 6 oz | 260 |
| Mozzarella, part-skim | 1 oz | 210 |
| Cheddar | 1 oz | 205 |
| Greek yogurt | 6 oz | 200 |
| American cheese | 1 oz | 195 |
| Feta cheese | 4 oz | 140 |
| Cottage cheese | 4 oz | 125 |
| Fortified food | Serving Size | Estimated calcium |
| Almond milk, rice milk or soy milk, fortified | 8 oz | 300 |
| Tofu, prepared with calcium | 4 oz | 205 |
| Orange juice fortified with calcium | 4 oz | 150 |
| Cereal, fortified | 8 oz | 100-1,000 |
| Source: International Osteoporosis Foundation | ||
Finally, in both men and women, osteoporosis could be linked to poor dietary consumption of minerals like calcium and lifestyle factors, but osteoporosis could be from a condition that prevents calcium absorption such as pancreatitis, celiac disease, or inflammatory bowel disorders such as Crohn’s disease or ulcerative colitis.
Chemotherapy, radiation, or medications such as steroids to treat a variety of conditions, such as asthma, can contribute to bone thinning.
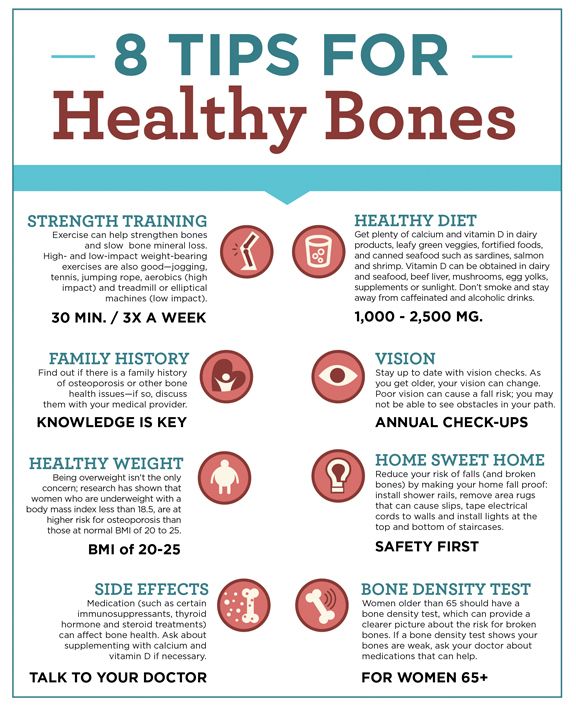
Another thought — avoid falls by checking your vision yearly and making sure your home is fall-safe.
Sources
Berkeley Wellness. Calcium Pills: Heartening News.
BMJ Open. Comparison of fracture risk using different supplemental doses of vitamin D, calcium or their combination: a network meta-analysis of randomized controlled trials.
ConsumerLab.com. Calcium supplements review.
Dr. Andrew Weil. Health & Wellness—Bone & Joint. Osteopenia.
Harvard Health Letter. How much calcium do you really need?
International Osteoporosis Foundation.
Journal of the American Medical Association. Association Between Calcium or Vitamin D Supplementation and Fracture Incidence in Community-Dwelling Older Adults. A Systematic Review and Meta-analysis.
National Institutes of Health, Office of Dietary Supplements: Calcium Fact Sheet for Consumers.
National Osteoporosis Foundation. Osteoporosis exercise for strong bones.
The Washington Post. Calcium and vitamin D supplements may not protect against bone fractures.
_______________________________
Food, Nutrition, and Your Health columnist Susan Burke March moved to Cuenca after 35 years as a Registered and Licensed Dietitian and Certified Diabetes Educator in the United States. She currently serves as the Country Representative from Ecuador for the Academy of Nutrition and Dietetics.
Susan helps people attain better weight and health, and reduce the risk of heart disease, diabetes, and other conditions that can be improved with smart lifestyle modifications. Contact her at SusantheDietitian@gmail.com.