Should you get your DNA tested to determine your diet?
If you want to avoid obesity, should you have your DNA tested to learn what is the best diet for you?
The answer is… no.
Well, you can, if you want to. As advertised in a popular ‘gringo’ online forum, you can spend hundreds of dollars and send a sample out to Spain then wait for eight weeks or so for the results. The price quoted doesn’t include shipping costs, so be prepared to fork over big bucks. Based in Spain, 24 Genetics offers a bunch of different bundled tests, ranging from ancestry to skincare, to talent and personality (?), to “nutrigenomics.”
Nutrigenomics, or nutritional genomics, is defined as a science studying the relationship between human genome, nutrition, and health.
24 Genetics advertises buying their test to allow your doctor to “tailor a diet to your needs,” but is there any evidence that knowing your DNA can reduce your risk for obesity? Is it necessary to know your DNA to lower your risk for any disease associated with diet, such as heart disease, hypertension, type 2 diabetes, arthritis, depression… cancer?
As reported in NutritionAction.com, one of the genetic markers that genetic companies claim will help you choose the right diet is the FTO gene. People with a varient of the FTO gene are more likely to be overweight or have obesity. And? What will that tell you?
John Mathers, director of the Human Nutrition Research Centre at Newcastle University in England, looked at eight weight loss studies (9,500 volunteers) with overweight or obesity and found that people lost weight just as effectively whether they had or didn’t have the risk variant for that gene. This means that genes are not always predictive, and people can lose weight even if they carry the risk variant.
And noted: researchers have found 97 gene variants linked to weight, but together, they only explain roughly three percent of the differences in weight between people.
And what about testing to see how food affects you? Do you have to send away your sample to know if you have gas, diarrhea, or bloating after drinking milk? Or do you avoid dairy products? Do you eschew coffee after breakfast because you know that afternoon latte will keep you up at night? Do you need a DNA test to ascertain your sensitivity to caffeine?
Nutrition Action writes, “An ordinary checkup can tell you if your blood pressure, blood sugar, triglycerides, or weight is high or if your HDL or vitamin D is low. What’s more, “for type 2 diabetes, body weight, and cardiovascular disease, non-genetic risk factors are much more important than your genetic risk,” says Cecile Janssens, research professor of epidemiology in the Rollins School of Public Health at Emory University. She’s talking about your blood pressure, blood sugar, HDL, etc.”
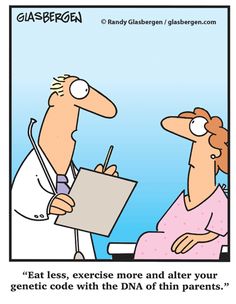
‘We’ve isolated the obesity gene down to one of these two.’
Non-genetic risk factors. What are those? These are risk factors that you can control. They don’t control you. What you eat, how much you eat, how you sleep, how much you sleep, how active you are, how much stress you have. Well… stress is a hard one. Let’s not stress about that.
And what about diet? Can your DNA tell you what you “should” be eating to stay healthy? To keep from gaining weight? What is the best diet for you to lose weight?
As reported in Scientific American, “DNA testing won’t guide dieters to the weight-loss regimen most likely to work for them. Despite some earlier studies claiming that genetic variants predict whether someone has a better chance of shedding pounds on a low-carbohydrate or a low-fat diet, and despite a growing industry premised on that notion, the most rigorous study so far found no difference in weight loss between overweight people on diets that “matched” their genotype and those on diets that didn’t.
The findings make it less likely that genetics might explain why only some people manage to lose weight on a low-carb diet like Atkins and why others succeed with a low-fat one (even though the vast majority of dieters don’t keep off whatever pounds they lose). Unlike cancer treatments, diets can’t be matched to genotype, the new study shows.”
 Are any genetic health tests worthwhile? A very recent report in Reuters (January 2020) isn’t positive.
Are any genetic health tests worthwhile? A very recent report in Reuters (January 2020) isn’t positive.
“Many people worry about inheriting health problems from their parents, but a new approach to analyzing genetic contributions to disease risk suggests that for most diseases, commercial DNA tests are not the best way to assess the odds.
For the study, researchers analyzed data from almost 600 earlier studies that found associations between common variations in the DNA sequence, known as single-nucleotide polymorphisms (SNPs), and more than 200 medical conditions. Usually, genetics explained no more than 5%-10% of the risk for several common ailments including certain cancers, diabetes and Alzheimer’s.
“Most common, chronic diseases have little to do with genetics or to do with your parents or the genes you inherited from them,” said senior study author David Wishart, a researcher at the University of Alberta in Canada.
“If you are worried about developing a disease, genetic testing won’t tell you much – unless you have a strong family history of a certain disease (multiple parents, siblings, aunts and uncles are afflicted),” Wishart said in an email.
The study found some exceptions, where genetics clearly do play a more powerful role, accounting for up to about half of the risk for diseases like Crohn’s, celiac and macular degeneration, Wishart noted.
“Despite these rare exceptions, it is becoming increasingly clear that the risks for getting most diseases arise from your metabolism, your environment, your lifestyle, or your exposure to various kinds of nutrients, chemicals, bacteria, or viruses,” Wishart said.”
Yes, you can find out your ancestry, possibly get some surprises or reinforce what you know about your family ties, but what about your risk for obesity? Uh… do you need a DNA test for that? Can you change your risk for disease by changing your diet?
Of course, you can! There are hundreds of studies of thousands of people that conclusively define what dietary patterns increase your risk for disease. Ditching refined carbohydrates, sugary beverages, deep-fried foods, and excess alcohol is really good medicine. This year, as in previous years, the Mediterranean-type diet is on top for an eating pattern and lifestyle that people can adopt with the assurance that even if you may have risk factors for disease, you are doing your very best to live healthier, longer lives. The ‘lifestyle’ means that it includes regular activity, a decent amount of sleep, and reducing stress deliberately (activity helps).
Any registered dietitian, or really, any person who pays attention to credible scientific research can tell you how to reduce your risk for obesity. Without spending hundreds of dollars on genetic testing. Or additional money on dietary supplements. Eating to live, not living to eat. And enjoying it.

The Mediterranean diet promotes the consumption of vegetables and fruits in addition to oily fish, olive oil, red wine, lean meats, nuts, and low-fat dairy products. It has been known since the late 1950s that it does offer cardioprotective benefits and several large and not so large studies have confirmed these findings since.
Learn more about the Mediterranean-type eating pattern here.
It’s generally accepted that the folks in countries bordering the Mediterranean Sea live longer and suffer less than most Americans from cancer and cardiovascular ailments. The not-so-surprising secret is an active lifestyle, weight control, and a diet low in red meat, sugar and saturated fat and high in produce, nuts and other healthful foods. The Mediterranean Diet may offer a host of health benefits, including weight loss, heart and brain health, cancer prevention, and diabetes prevention and control. By following the Mediterranean Diet, you could also keep that weight off while avoiding chronic disease.
Sources:
Nutrition Action. When nutrition gets personal.
Reuters. Genetic markers not very good for predicting disease risk.
Scientific American. Matching DNA to a diet does not work.
____________________________
Food, Nutrition, and Your Health columnist Susan Burke March moved to Cuenca after working for more than 25 years as a Registered and Licensed Dietitian and Certified Diabetes Educator in the United States. She currently serves as the Country Representative from Ecuador for the Academy of Nutrition and Dietetics.