Antibiotics — a miracle drug that’s changed direction?
What was life like in Ecuador prior to antibiotics?
In a word: short. For people with bacterial infections, life was cruel… but of course, not just in Ecuador. As described by the American Chemical Society, “Before [penicillin was introduced] there was no effective treatment for infections such as pneumonia, gonorrhea or rheumatic fever. Hospitals were full of people with blood poisoning contracted from a cut or a scratch, and doctors could do little for them but wait and hope.”
treatment for infections such as pneumonia, gonorrhea or rheumatic fever. Hospitals were full of people with blood poisoning contracted from a cut or a scratch, and doctors could do little for them but wait and hope.”
I thought of this recently, while attending a viewing of a poignant documentary titled, “An Unknown Country” at the Museo Pumapungo. The story of European Jews who escaped Nazi persecution to find refuge in Ecuador, the film “follows the exiles’ perilous escape and difficult adjustment as they remade their lives in what was for them an exotic, unfamiliar land.” Ecuador was almost unknown by most of the European Jews looking for escape and refuge from certain death. The film reveals why Ecuador, a small country of barely three million people and few resources, granted asylum to the refugees and saved thousands of lives. View the film on PBS.org.

Guayaquil at the turn of the 20th Century.
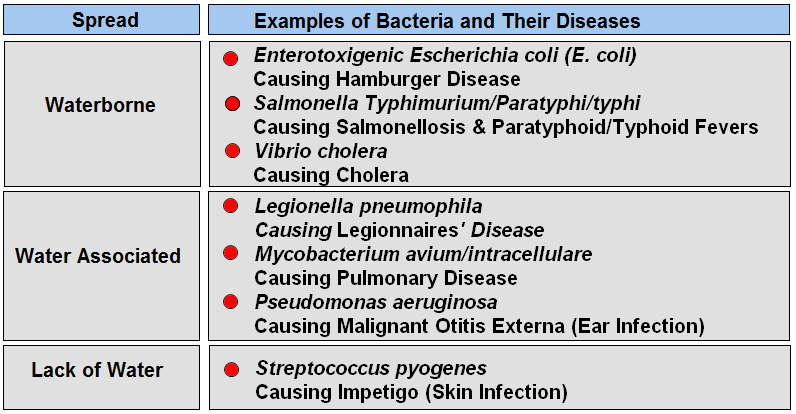
The Jews all arrived by boat and landed near Ecuador’s west coast, in Salinas or La Libertad. No piers existed, so they were ferried by small boats to the port city of Guayaquil. Bacterial diseases plagued the new arrivals as well as everyone else, including hepatitis, typhoid, and tuberculosis, and diarrhea from any number of bugs. Cholera, diphtheria…tetanus, typhus, syphilis, and gonorrhea — all bacterial diseases without any reliable treatment. Parasites and amoeba from contaminated food and/or water were common. Besides bacteria, protozoan diseases such as malaria were rampant. Without vaccination, viruses including measles, mumps, rabies (human and animal), polio, yellow fever, and influenza assured life expectancy at birth was around thirty-five years.
[Today, Ecuador ranks 49 in life expectancy — 76.5 years (male 74.1, female 78.6). There are no bacterial causes in the top 30 leading causes of death except for tuberculosis, at number 29, a bacterial infection — caused by Mycobacterium tuberculosis, acquired by breathing contaminated air droplets, or by ingesting unpasteurized milk products contaminated with Mycobacterium bovis. Diarrheal diseases are ranked at 36. Deaths from coronary heart disease and diabetes rank first and second, akin to most Western countries, linked to lifestyle and environmental factors.]
Until the discovery of penicillin the simplest cut or wound could mean death, any form of surgery was considered risky, and mothers and their children commonly died from postnatal infections. As reported in PastMedicalHistory.co.uk, “All this changed in 1928 though, with the groundbreaking work of Sir Alexander Fleming and that of Sir Howard Florey, Sir Ernst Boris Chain, and Norman Heatley after him.

Sir Alexander Fleming, Scottish biologist, pharmacologist, and botanist who discovered Penicillin. Credit: Fame Images
In 1928 the bacteriologist Fleming was working in the inoculation department of St. Mary’s Hospital in London, England. He had been on a summer vacation in Scotland and returned to find a messy lab bench with a Staphylococcus culture plate that had been contaminated with a mold. Initially, he thought that this was just a spoiled experiment, but on closer inspection, he noticed that no bacteria was growing near to the mold. The mold had created a bacteria-free circle around itself.
The discovery of penicillin marked the start of the development of an important group of medicines called antibiotics — special bacteria-killing drugs. Known as a broad-spectrum antibiotic because it kills a wide range of bacteria, penicillin itself would become responsible for killing the different bacteria responsible for many serious human infections — for example, tonsillitis, pharyngitis, bronchitis and pneumonia.
However, it took a dozen years after the substance’s initial discovery before penicillin was ready to be widely used as a medicine. In 1940 two researchers at the University of Oxford, Sir Howard Florey and Sir Ernst Boris Chain were planning a research project on natural bacterial killing substances. Using Fleming’s 10-year-old research, they decided to investigate the antibacterial properties of the penicillin substance that Fleming had discovered. In early summer 1940, the researchers infected 50 mice with deadly Streptococcus. Half were inoculated with penicillin, the rest left untreated. All the mice that had received penicillin lived and stayed healthy, and all untreated mice died from infection-caused sepsis.
Human trials were next, but producing penicillin proved very difficult. It took 2,000 liters of mold culture fluid to obtain enough pure penicillin to treat a single case of sepsis in a person.
Not until September of 1940 was a human treated — a man working in his rose garden was nicked in the face by a thorn. The scratch was infected with streptococci and staphylococci, and the infection quickly spread to his eyes and scalp. Treatment with sulfa drugs, commonly used at the time, failed — by the time Florey and Chain heard about the case the patient had seriously infected abscesses in the eye, lungs, and shoulder.
The hospital treating the patient agreed to a trial of the new “purified” penicillin, and after five days of injections, the patient began to recover. Unfortunately, there was not enough pure penicillin to continue treatment — the infection was not eradicated — and the patient ultimately died.

A technician preparing penicillin – 1943. Credit: PastMedicalHistory.co.uk
So, this major hurdle remained — how to produce enough purified penicillin to successfully eradicate bacterial infections in humans. As PastMedicalHistory.co.uk reports, “At the time World War II was raging and there was an enormous need for antibiotics for both soldiers and the public.” Florey and Heatley traveled to the U.S.A. to work with American scientists in Peoria, Ill. Along with the American team, they developed the means of synthetically mass producing what became known as “the wonder drug.” But it was a long and tortuous process. As reported by the ACS, “”The mold is as temperamental as an opera singer, the yields are low, the isolation is difficult, the extraction is murder, the purification invites disaster, and the assay is unsatisfactory.” But they succeeded. In 1949, Florey observed, “too high a tribute cannot be paid to the enterprise and energy with which the American manufacturing firms tackled the large-scale production of the drug. Had it not been for their efforts there would certainly not have been sufficient penicillin by D-Day in Normandy in 1944 to treat all severe casualties, both British and American.” Read more here.
Penicillin was a critical factor in keeping soldiers on the battlefield. Infection from illnesses and from battle wounds had always been the biggest killer, not the battle per se. In World War I, the death rate from bacterial pneumonia was 18 percent. In World War II, it fell to less than one percent.
 Are humans resistant to penicillin? No, the bacteria are.
Are humans resistant to penicillin? No, the bacteria are.
According to the Visual Capitalist, “For most of civilized history, life expectancy fluctuated in the 30 to 40-year range.
Child mortality was all too common, and even for those that made it to adulthood, a long and healthy life was anything but guaranteed. Sanitation was poor, disease was rampant, and many medical practices were based primarily on superstition or guesswork.
By the 20th century, an explosion in new technologies, treatments, and other science-backed practices helped to increase global life expectancy at an unprecedented rate.
From 1900 to 2015, global life expectancy more than doubled, shooting well past the 70-year mark.”
It is estimated that antibiotics have saved more than 200 million lives. However…
In 1945, Fleming predicted that the overuse of penicillin might lead to bacterial resistance and by the mid-1950s the first resistant strains appeared — doctors were prescribing it so much that some bacteria learned to “resist” the drug. The more antibiotics are used, the quicker that bacteria can ‘learn’ to change, which is why it is important that antibiotics are used properly.
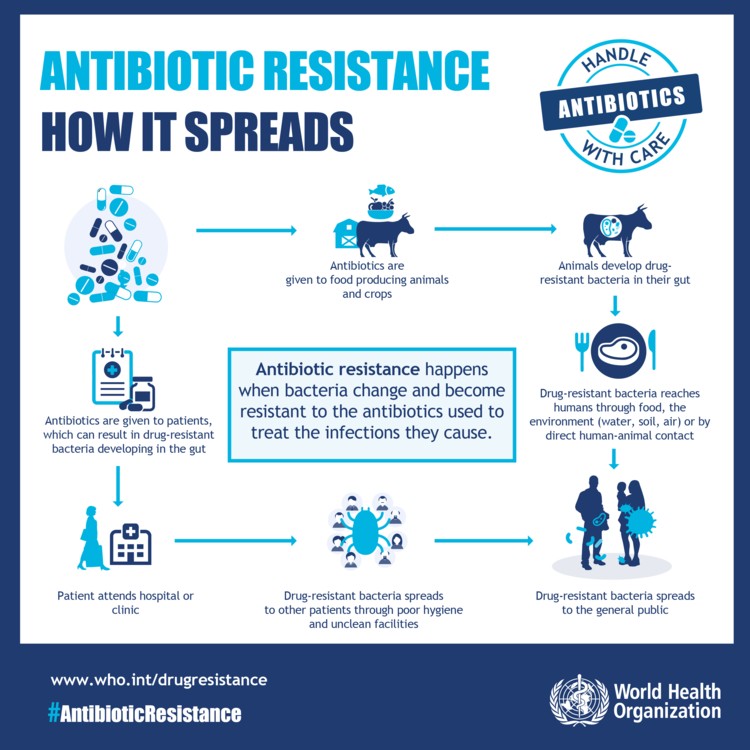
Health experts say that doctors may prescribe them unnecessarily, while many doctors say that patients demand them and don’t really need them. Antibiotics do not work on viral infections such as colds and influenza, and research shows that often coughs and sore throats and many mild bacterial infections will improve without antibiotics.
According to the World Economic Forum, “Antibiotic-resistant bacteria have become a serious threat to global health. Organizations and institutions around the world, including the World Health Organization (WHO), the United Nations (UN) and many governments, have undertaken joint efforts to prevent antibiotic resistance and they are aware they are fighting against time. There is no question that without serious cooperative action, simple infections that were easily treated with antibiotics in the past could become lethal. In short, without serious attention to this issue, our current healthcare procedures are too weak to win the war against antibiotic-resistant bacteria.”
According to the World Health Organization:
- Antibiotic resistance is one of the biggest threats to global health, food security, and development today.
- Antibiotic resistance can affect anyone, of any age, in any country.
- Antibiotic resistance occurs naturally, but misuse of antibiotics in humans and animals is accelerating the process.
- A growing number of infections – such as pneumonia, tuberculosis, gonorrhea, and salmonellosis – are becoming harder to treat as the antibiotics used to treat them become less effective.
- Antibiotic resistance leads to longer hospital stays, higher medical costs and increased mortality.
Prevention and control
Antibiotic resistance is accelerated by the misuse and overuse of antibiotics, as well as poor infection prevention and control. Steps can be taken at all levels of society to reduce the impact and limit the spread of resistance.
Individuals
To prevent and control the spread of antibiotic resistance, individuals can:
- Only use antibiotics when prescribed by a certified health professional.
- Never demand antibiotics if your health worker says you don’t need them.
- Always follow your health worker’s advice when using antibiotics.
- Never share or use leftover antibiotics.
- Prevent infections by regularly washing hands, preparing food hygienically, avoiding close contact with sick people, practicing safer sex, and keeping vaccinations up to date.
- Prepare food hygienically, following the WHO Five Keys to Safer Food (keep clean, separate raw and cooked, cook thoroughly, keep food at safe temperatures, use safe water and raw materials) and choose foods that have been produced without the use of antibiotics for growth promotion or disease prevention in healthy animals.
Policymakers
To prevent and control the spread of antibiotic resistance, policymakers can:
- Ensure a robust national action plan to tackle antibiotic resistance is in place.
- Improve surveillance of antibiotic-resistant infections.
- Strengthen policies, programs, and implementation of infection prevention and control measures.
- Regulate and promote the appropriate use and disposal of quality medicines.
- Make information available on the impact of antibiotic resistance.
Health professionals
To prevent and control the spread of antibiotic resistance, health professionals can:
- Prevent infections by ensuring your hands, instruments, and environment are clean.
- Only prescribe and dispense antibiotics when they are needed, according to current guidelines.
- Report antibiotic-resistant infections to surveillance teams.
- Talk to your patients about how to take antibiotics correctly, antibiotic resistance and the dangers of misuse.
- Talk to your patients about preventing infections (for example, vaccination, hand washing, safer sex, and covering nose and mouth when sneezing).
Healthcare industry
To prevent and control the spread of antibiotic resistance, the health industry can:
- Invest in research and development of new antibiotics, vaccines, diagnostics and other tools.
Agriculture sector
To prevent and control the spread of antibiotic resistance, the agriculture sector can:
- Only give antibiotics to animals under veterinary supervision.
- Not use antibiotics for growth promotion or to prevent diseases in healthy animals.
- Vaccinate animals to reduce the need for antibiotics and use alternatives to antibiotics when available.
- Promote and apply good practices at all steps of production and processing of foods from animal and plant sources.
- Improve biosecurity on farms and prevent infections through improved hygiene and animal welfare.
Sources:
An Unknown Country. PBS.org.
American Chemical Society. Discovery and Development of Penicillin.
BBC.co.uk. 90 years since discovery of penicillin: Sir Alexander Fleming’s great accident.
Guzman, Jose R., et al. Infectious Disease in Ecuador.
International Association for Medical Assistance. IAMAT. Ecuador for Specific Travelers: Tuberculosis.
PBS.org. The real story behind penicillin.
PewTrusts.org. The Fight Against Superbugs: 5 Priorities for 2019.
VisualCaptitalist.com. The 50 most important life-saving breakthroughs in history.
World Economic Forum. How we can win the war against antibiotic resistance.
World Health Organization. Antibiotic resistance.
WorldLifeExpectancy.com. World Health Rankings: Ecuador: Life Expectancy.
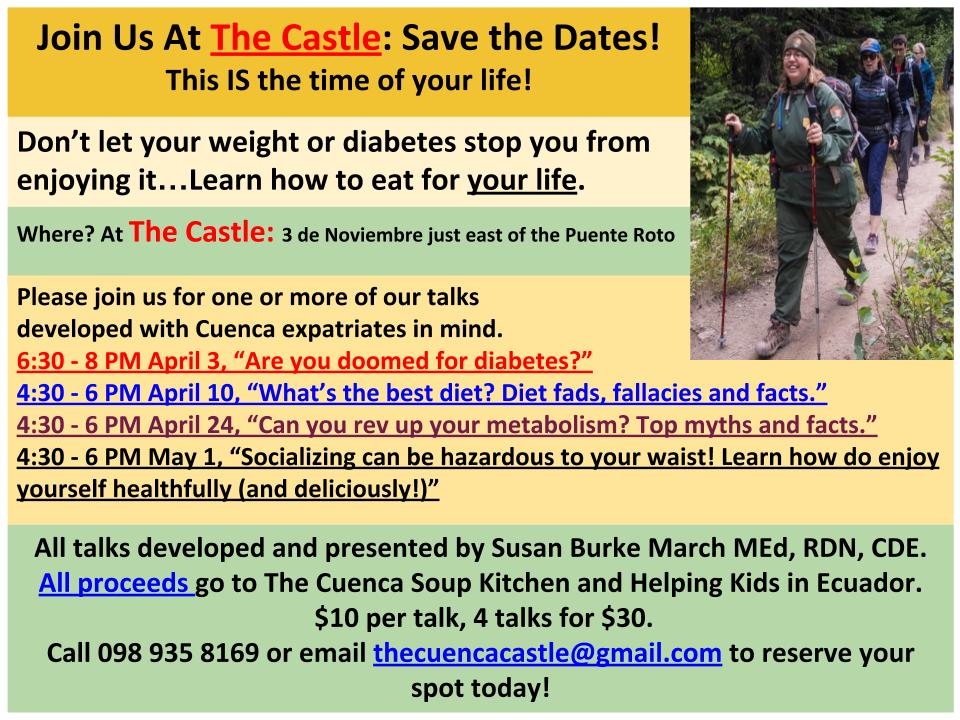 Susan Burke March, a Cuenca expat, is a Registered and Licensed Dietitian, a Certified Diabetes Educator who specializes in smart solutions for weight loss and diabetes-related weight management. She is the author of Making Weight Control Second Nature: Living Thin Naturally—a fun and informative book intended to liberate serial dieters and make healthy living and weight control both possible and instinctual over the long term. Have a question for Susan? Email SusanTheDietitian@gmail.com
Susan Burke March, a Cuenca expat, is a Registered and Licensed Dietitian, a Certified Diabetes Educator who specializes in smart solutions for weight loss and diabetes-related weight management. She is the author of Making Weight Control Second Nature: Living Thin Naturally—a fun and informative book intended to liberate serial dieters and make healthy living and weight control both possible and instinctual over the long term. Have a question for Susan? Email SusanTheDietitian@gmail.com